Fetal Surgery for Congenital Heart Defects
Even before they are born, infants with some congenital heart defects may be eligible for surgery with fetal interventions at Columbia.
The Fetal Cardiac Intervention Program, the first of its kind in New York state, opened last year within the fetal cardiac program.
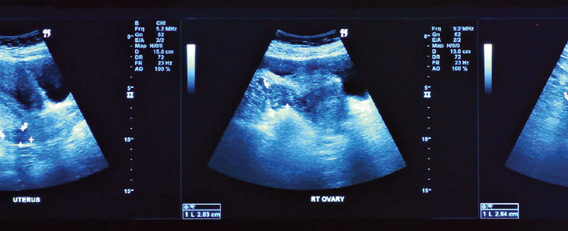
“For most cases of congenital heart defects, fetal interventions are not feasible because of anatomical limitations or because the diagnosis was made too late,” says Stéphanie Levasseur, MD, assistant professor of pediatrics, who directs the fetal cardiac program. “The patients are seen by the fetal cardiologist and maternal fetal medicine team to assess candidacy for the procedures.”
Fetal interventions may be an option if a patient has aortic stenosis evolving to hypoplastic left heart syndrome, pulmonary atresia, or some forms of hypoplastic left heart syndrome. For these cases, Columbia pediatric cardiologists can modify the fetal heart with balloons or stents delivered via a catheter through the womb and into the fetus. “The goal is to improve outcomes and minimize invasive interventions after birth,” says Dr. Levasseur.
The most common fetal cardiac procedure–aortic balloon valvuloplasty–is used for patients with an obstructed aortic valve that causes further heart damage. Physicians expand the valve with an inflatable balloon in an effort to prevent the development of hypoplastic left heart syndrome, when the left side of the heart weakens and cannot pump blood properly.
Similarly, an inflatable balloon also can open an obstructed pulmonary valve that is not working properly in fetuses with a condition called pulmonary valve atresia. However, the condition is more variable than its counterpart on the left side of the heart, and fetal pulmonary balloon valvuloplasty is reserved for select patients.
While balloon valvuloplasty is used to prevent heart damage from developing, the goal of the third procedure offered by the team is to improve survival. Fetal atrial septal stent implantation is for patients who have already developed hypoplastic left heart syndrome and whose foramen ovale has closed prematurely. In such patients, birth causes a circulation crisis and mortality is high even at experienced centers that are prepared to perform immediate surgery.
Implanting a stent to create an opening between the two atria may increase the odds of survival. “The success of invasive fetal interventions requires the collaboration of an experienced, multidisciplinary team,” says Matthew Crystal, MD, associate professor of pediatrics and director of the fetal cardiac intervention team at NewYork-Presbyterian. “This includes high-risk obstetrics, fetal and interventional cardiology, and anesthesia, which were well-established at Columbia when we began the program.
“As the field progresses, we hope to be able to offer procedures earlier and with greater success,” says Dr. Crystal.
More information is available at www.columbiaobgyn.org/services/fetal-cardiology. Referrals can be requested by calling the Center for Prenatal Pediatrics at 212-305-3151.
- Log in to post comments