Preventing Suicide: Genetic Studies, Screenings, Apps
Randy P. Auerbach, PhD, associate professor of psychiatry
Madelyn Gould, PhD, the Irving Philips Professor of Epidemiology (in Psychiatry) at CUMC
J. John Mann, MD, the Paul Janssen Professor of Translational Neuroscience (in Psychiatry and in Radiology)
Kelly Posner, PhD, clinical professor of medical psychology (in psychiatry)
Barbara Stanley, PhD, professor of medical psychology (in psychiatry) at CUMC
No one can explain why the suicide rate in the United States has gone up nearly every year of this century—despite decreases worldwide over the same period—but experts agree that suicide is preventable.
Suicide attempts in the United States are also increasing. In contrast to these two statistics—increases in suicides and suicide attempts—more people than ever are seeking help, effective therapies exist, and prescriptions for antidepressants and mood stabilizers are at all-time high numbers. None of this has stanched the tide.
“All of us have lost people in our lives,” says Randy Auerbach, PhD, an expert in adolescent depression and suicide who also co-directs the World Health Organization World Mental Health International College Student Initiative. “But it’s different when you lose someone by their own hand. You feel for the family. You also feel for the individual, how much this person must have been suffering, how painful each day of their life must have been where they felt this was their best option that day. It’s something we feel shapes the type of work we do.”
 Randy Auerbach
Randy AuerbachHe also has received federal funding to lead the NIMH study called Mobile Assessment for the Prediction of Suicide (MAPS). The study uses smartphones to collect data from 200 high-risk adolescents, most of whom have a history of suicidal thoughts or actions, to identify patterns in behavior known to have some connection to suicide.
The Silvio O. Conte Center for Suicide Prevention at Columbia and the New York State Psychiatric Institute also focuses on prevention efforts by learning about the fundamental causes of suicide. Funded by the NIMH, the center brings together clinical, laboratory, brain imaging, and big data analytic capabilities to probe how genes and childhood adversity—nature and nurture—combine to create a predisposition to suicidal behavior.
The center is led by J. John Mann, MD, a pioneering suicide researcher who received the 2019 Lifetime Achievement Award from the American Foundation for Suicide Prevention. One of the center’s goals is development of a model to predict suicide risk, recognizing that not all people with depression die by suicide.
One avenue of research is the study of the heritable component to suicide. The Conte Center is part of a worldwide consortium of investigators trying to identify specific genes that may contribute to suicide risk. “It will take time, but we will get there,” says Dr. Mann. “When you combine that with clinical information about people who have a psychiatric illness, we should be able to narrow it down to the subgroup most at risk for suicide. They are the ones who really need protection and focus in terms of treatment and prevention.”
But even identifying someone at risk of suicide doesn’t identify everyone who is in jeopardy. “We understand suicide attempters are more depressed and more impulsive,” says noted suicide researcher Barbara Stanley, PhD, “but we haven’t been able to walk up really close to the suicide event itself. It’s like trying to predict who will have a myocardial infarction the week or days before it occurs. We are not very good at identifying near-term risk.”
 Barbara Stanley
Barbara Stanley
Mobile Assessment for the Prediction of Suicide
Suicide prevention experts want Tim Cook to get up in front of Apple customers one day and tell them how the iPhone is going to help prevent suicide.
That’s where the MAPS project may help. Tone of voice. Language use. Quality of sleep. How often one reaches out to friends or leaves the house. The contours of a smile in a picture. Many of these behavioral markers are known to be associated with depression and suicide. Dr. Auerbach hopes to use the data collected from smartphones to create computational models that capture how suicide risk is expressed in real time. The NIMH has just awarded the Conte Center additional funding to test this approach in the patients being studied and link the mobile app findings to the brain imaging and stress lab measurements used by the Conte Center.
“The ultimate advantage is that if we’re able to utilize this assessment in real time, we’ll be able to identify features that relate to transitions between suicidal thinking and behaviors,” says Dr. Auerbach. “We can then start to think in creative ways about how to deliver ‘just-in-time’ interventions—not necessarily where somebody is ultimately going to make a decision to end their life but ideally when they start wading into a territory where they’re at risk.”
Self-reporting is a limitation of many mental health studies. Subjects aren’t always transparent. They can be mistaken. Even the most mindful might not be able to tell when they are in a precarious state. MAPS sidesteps many of these obstacles by requiring minimal user interaction. The app runs in the background. Subjects have periodic check-ins, to see how they might be feeling, but the true value is in the data they provide by going about their lives, material from which predictive algorithms can be made.
 Janis Cutler
Janis CutlerLearning about suicide risk and prevention is part of the coursework at VP&S from the first semester’s “Foundations of Clinical Medicine” course.
By their second semester, students take a psychiatric medicine course taught by Janis Cutler, MD, professor of clinical psychiatry. In one session of the course, standardized patients act out symptoms of depression and students screen them for suicidal ideation. Their small group preceptors guide them in techniques for talking to patients about suicide. “Students struggle at first with asking direct questions,” says Dr. Cutler. “They worry about being impolite or giving a patient harmful ideas. Asking the right questions is important in getting a patient to express suicidal thoughts.”
In time for major clinical year, students learn to assess patients for suicidality when giving bad news to patients. All are required to complete a five-week psychiatry clerkship in hospital and clinic settings, where they rotate in a psychiatric emergency room and interview at least one patient suffering from suicidal ideation. At the end of medical school, in the Ready 4 Residency course, students participate in a session that provides guidance on when to hospitalize suicidal patients.
“Suicide is a global public health crisis,” says Jonathan Amiel, MD, associate professor of psychiatry and senior associate dean for curricular affairs at VP&S. “Our medical school is committed to ensuring graduates are prepared to do their part in helping to prevent suicide by learning how to identify at-risk patients in medical settings and helping those who have attempted or are at risk for suicide to access quality care.”
— Rose Spaziani
Dr. Auerbach aims for findings that are reliable and replicable, but to what extent will insights gleaned from teenage subjects be applicable to other demographics? “The potential is enormous,” says Dr. Mann, who also works on the project. “It’s unproven technology, but it has a lot of common sense opportunity. By combining all the other things we’re doing with our patients, we’re enriching the information we are collecting. One day we want Tim Cook to get up there in front of Apple customers and tell them not how the iPhone is going to be good for their cardiovascular health, but how it’s going to help prevent suicide.”
More Traditional Approaches
As high tech as MAPS is, Columbia also has been at the forefront of suicide prevention efforts with the Columbia-Suicide Severity Rating Scale (C-SSRS), a simple but proven effective questionnaire to assess suicidality. Based on decades of research, it has saved lives since it was introduced in 2007. The Columbia Protocol, as it is known, is considered the gold standard in assessing suicide risk and has been adopted by schools, hospitals, jails, and military organizations in more than 45 countries.
“We knew that if we wanted a real change, we needed a simple common method for asking about suicidal thoughts and behaviors that everyone can use,” says Kelly Posner, PhD, who leads the work. “With the C-SSRS, we are well on our way to making the language of asking about suicide accessible to everyone and suicide screening routine across all public health settings.”
Dr. Stanley helped to create an intervention for use once patients have been identified as being at risk by tools like the C-SSRS. The Safety Planning Intervention is helpful in managing the dangerous period post-discharge following hospitalization or an ED visit for a suicide attempt or because of suicidal thoughts. Dr. Stanley’s research has found that a simple safety plan created with the patient, which details warning signs, coping strategies, and resources to be used if suicidal thoughts or feelings return, can give that person a sense of control in vulnerable moments. A 2018 study on suicidal patients in VA hospitals found that a safety plan, along with follow-up calls from a clinician 72 hours after discharge, cut the odds of that patient re-attempting suicide by 50% in the next six months. Twice as many sought mental health care when they were distressed if they left the hospital with the safety plan.
Research has laid the groundwork for the launching of a three-digit national hotline number—988—as recommended by the Federal Communications Commission.
The Media’s Role in Prevention
Another area of Columbia suicide prevention research is led by psychiatric epidemiologist Madelyn Gould, PhD, MPH. In three decades of research that has been continuously funded by the Centers for Disease Control and Prevention, the National Institute of Mental Health, and the Substance Abuse and Mental Health Services Administration, Dr. Gould has shown how and why suicide is contagious and elucidated the news media’s role in promoting—or stemming—the spread of suicidal behavior.
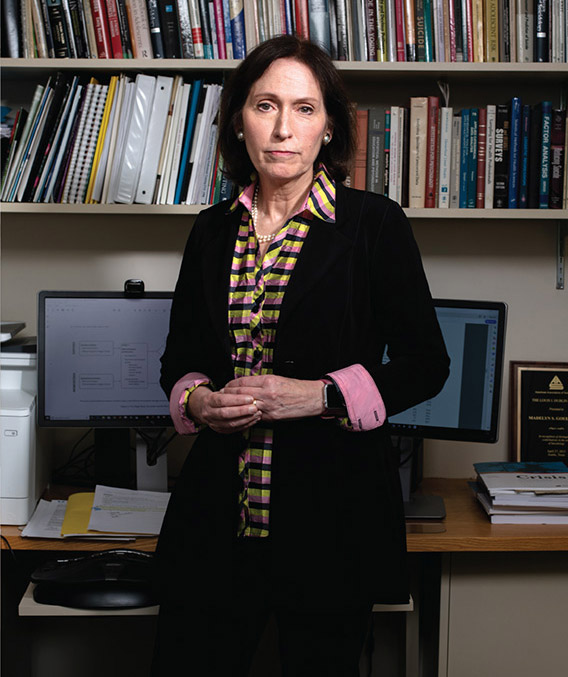 Madelyn Gould
Madelyn GouldShe has contributed to the CDC’s community response plan for suicide clusters and recommendations to optimize media reporting of suicide and has been a member of national and international workgroups that update media recommendations.
She currently leads the evaluation of the National Suicide Prevention Lifeline, the national network of telephone crisis services that has emerged as an important part of suicide prevention programs. Her findings have led to improvements in services, including an initiative to have crisis centers offer and provide clinical follow-up to suicidal hotline callers. The evaluation findings have also laid the groundwork for the launching of a three-digit national hotline number (988), as recommended by the Federal Communications Commission in August of 2019. In November, a team of senators introduced a bipartisan bill to make 988 the three-digit number to reach the National Suicide Hotline.
“The 2001 U.S. National Strategy for Suicide Prevention barely mentioned crisis hotlines,” says Dr. Gould, “but the 2010 National Action Alliance for Suicide Prevention prominently referenced Lifeline and telephone crisis services as important to the national strategy. Now, media reports of suicides routinely provide a suicide hotline number.”
Challenges Remain
From cutting-edge explorations of the genetic and neurochemical roots of suicide to common sense methods to identify those at risk, Columbia investigators are contributing to the body of research that could make a difference. “We have more people working on suicide prevention research than anywhere in the world,” says Dr. Mann.
Suicide is the 10th leading cause of death across all age groups.
In 2017, more than 47,000 Americans died by suicide,a 31% increase over 2001.
One person dies by suicide every 11 minutes.
Suicide is the second leading cause of death among people age 10 to 34.
Suicide is the fourth leading cause of death among people age 35 to 54.
The number of suicides in 2017 was more than double the number of murders.
* Centers for Disease Control and Prevention
Among the challenges that remain: Some people who die by suicide never come into contact with the health care system at all because they are uninsured, or underinsured, or they live in remote areas.
The largest challenge, though, is stigma. Unlike HIV or cancer, suicide has not prompted massive activism or increased funding for research or treatment. People continue to suffer in silence, and when a suicide ends one person’s pain, it transfers that pain to many more people who are left behind to mourn the loss. Reducing the stigma associated with suicide is on the agenda of everyone focused on suicide prevention. “Stigma is a huge barrier to treatment of all mental illnesses,” says Dr. Mann. “Breaking down the barrier will help identify people who suffer in silence so we can get them the care they need and it will help patients understand that they have an illness that is not their fault and needs to be treated like any other type of illness.”
National Suicide Prevention Lifeline
24/7 free and confidential support for people in distress, prevention and crisis resources for you or your loved ones, and best practices for professionals.
800-273-TALK (8255)
- Log in to post comments


