Goal of MD-PhD Student Research: Improve Patient Care
 Ben Schrank. Photo by Susan Conova.
Ben Schrank. Photo by Susan Conova.Graduate student Ben Schrank’s paper in Nature started with a hunch. Dr. Schrank, a student in Columbia’s MD-PhD program, and his mentor Jean Gautier, PhD, were looking for new proteins that might be involved in DNA repair. “If you’re able to inhibit DNA repair, you could make cancer treatments more effective,” says Dr. Schrank, who received his PhD degree in November 2018.
A mass spectrometry machine analyzed a batch of frog DNA and produced a list of more than 100 proteins that could potentially play a role. Two possibilities—Arp2/3 and actin—stood out to Dr. Schrank and Dr. Gautier, professor of genetics & development in the Institute for Cancer Genetics, who has studied DNA repair for years.
“Our project was high risk, high reward,” says Dr. Schrank. “There was no precedent in the scientific literature that explained active roles for Arp2/3 and actin. It was a gamble on my part. Jean and I talked and he encouraged me to do the experiments.”
Those experiments revealed that Arp2/3 and actin are critical conductors of DNA repair. The proteins push the ends of broken DNA into clusters where repairs are made, and repair falters when damaged DNA can’t be moved.
Discoveries like this underscore the mission of Columbia’s MD-PhD program. Student trainees hone their research skills in the labs of faculty mentors, pursuing scientific findings that may be translated into clinical practice. The program matriculates 12 to 15 students per year, and the program currently has 104 MD-PhD students, from those in their first year to those in their final year of the program.
“The goal of the MD-PhD program is to train the next generation of biomedical leaders,” says Steven L. Reiner, MD, director of the MD-PhD program. “The curriculum emphasizes both clinical and scientific education, enabling our graduates to become research innovators and play a key role in the translation of scientific findings to clinical practice.”
Dr. Schrank submitted his research to Cell and spent eight months interacting with the journal’s editors and revising the draft before the paper was turned down. Rejection stung, but Dr. Schrank pressed on. The paper was strengthened through multiple revisions and was ultimately accepted by Nature with Dr. Schrank earning a first author credit.
Dr. Schrank plans a career in radiation oncology, an area closely tied to the research he has conducted. Since completing his clinical clerkships, he’s come to fully appreciate the thoughtful discussions happening at Columbia around patient care and research. “The conversations are not just about how we should treat patients,” he says. “They’re about why we’re providing this treatment for a patient. What’s the evidence for this treatment?” He believes the MD-PhD program is preparing him to go beyond practicing medicine to bring change to the field—and that change comes from knowing how to ask the right questions and find the answers in science.
“The beauty of research is it’s very autonomous,” says Dr. Schrank. “I came into the lab day and night. I had a list of experiments and ran them simultaneously. All of my experiments went into the paper.”
Building Resilience as a Research Scientist
MD-PhD students are expected to publish their work. The process can be grueling. There are no guarantees when conducting research. Aha moments are few and far between.
 Matthew Decker. Photo by Jeffrey Schifman.
Matthew Decker. Photo by Jeffrey Schifman.“The process of conducting research and turning it into a paper is long and a lot of it is out of your control,” says Matthew Decker, an MD-PhD student in the lab of Lei Ding, PhD, assistant professor of rehabilitation & regenerative medicine and of microbiology & immunology. “There are many ups and downs, but they’re also a valuable part of your training.”
In addition to publishing their research, MD-PhD students have to navigate a program that starts with medical school, then moves to the laboratory, and then back to medical school.
“MD to PhD is like switching to a different part of the brain but in an enjoyable way,” says Dr. Decker, who received his PhD in September 2018. “As a PhD student, you are creating new knowledge in a narrow field. As a medical student, you’re learning an incredible amount from a huge field. These are two different modes of learning but doing both gives you a great combination of skills invaluable to a doctor and research scientist.”
During the initial MD portion, students follow the same curriculum as traditional medical students but also rotate in labs to find the right research mentor. “I wanted to work with an investigator beginning his career,” Dr. Decker explains, “someone who would trust me with big ideas and projects.”
Dr. Decker studied how the body supports production of hematopoietic stem cells (HSCs), which give rise to all blood cells. With the help of machinery that can sort through tens of millions of cells, Decker discovered that a growth factor that keeps HSCs healthy is supplied by a surprising source, the liver. These findings could inform how HSCs are stimulated for therapeutic use and lead to improvements in bone marrow transplantation.
After 18 months of research, Dr. Decker began preparing a manuscript, which took another month. In the weeks after he submitted the manuscript to Nature and waited for feedback, he continued to conduct experiments and gather more data. The manuscript was turned down, so he submitted it again, this time to Cell, and received another rejection.
“One thing I’ve learned is that sometimes people will not be interested in the things you’re interested in and that’s not a reflection of the worth of your research,” says Dr. Decker.
He used the comments from the journals, as well as data from ongoing experiments, to improve the paper. Next time he submitted the research, it was accepted by Science.
Feeling of Freedom
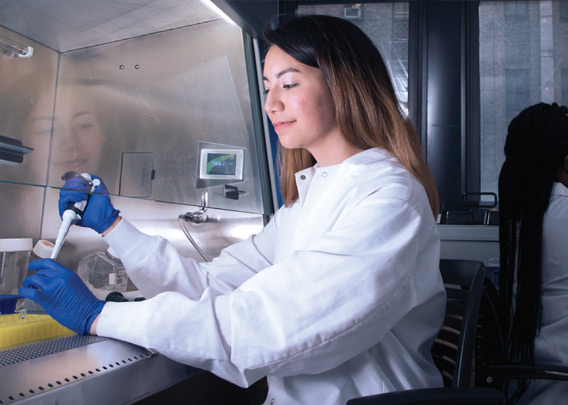 Heather Lee. Photo by Jeffrey Schifman.
Heather Lee. Photo by Jeffrey Schifman.Heather Lee, like Dr. Decker, is an MD-PhD student in Dr. Ding’s lab, where she has room to branch out. She is the only one in the lab investigating the behavior of genes within HSCs instead of examining their environment.
“It’s a great feeling to come to the lab and have your own project, decide the research questions, and then figure out how to answer them,” says Dr. Lee, who received her PhD in November 2019. “You can’t find these answers on the Internet.”
What Dr. Lee studies may one day impact treatments for leukemia and other types of blood diseases. She studies the factors that control HSCs: What causes them to generate more stem cells or go on a different path and develop into more mature cells. These processes often go awry in blood cancers.
In her paper in Nature Cell Biology, Dr. Lee identified a new factor—called m6a methylation—that pushes HSCs to become mature cells but is not needed once cells have matured. “Our study and others suggest it may be possible to develop m6A-targeted therapies against leukemia cells without damaging HSC function,” she says.
Though excited by the findings, she also experienced some uncertainty. Her research contradicted a long-held assumption among scientists that removing m6A alters gene expression; Dr. Lee found no such change.
“I had a moment of doubt,” says Dr. Lee, whose paper was rejected by two other journals before it was accepted for publication. “I questioned my research at first but ultimately I had to trust myself.”
Trusting her gut led Dr. Lee to science in the first place, combined with the example of her parents who were graduate students when they met. In college, Dr. Lee conducted research for three years in an immunology lab and planned to apply to medical school. Her faculty mentor encouraged her to consider an MD-PhD program, something she had not known existed. Going through the program has only solidified her interest in a career as a medical scientist.
“My goal is to have a career combining research and medicine,” says Dr. Lee. “The training in Columbia’s MD-PhD program opens a lot of doors to ask clinical and translational questions and those are skills that a lot of other people don’t have. Conducting biomedical scientific research provides useful information. What you find will help people in some way and you’re adding to this scientific community that’s trying to understand things better.”
- Log in to post comments

